Hello Friends!
After a long winter break (in SA +- from June to September) I am seriously back with a rather long and scientific article and info I found for you. That means we are getting to a new start with very serious diabetes business: The A1C! My count was 6.1 last time I checked (in June actually, going again in November).
I am on Insuline in the meantime, but since then my blood sugar control has improved. The injections are not as uncomfortable as I thought, especially when you call to mind the potentail alternatives! You probably know know how some people cringe at ' Twice a day into the belly.....?'
So I have reason to be quite proud of myself. I used the -not too bad this year- winter to hybernate and contemplate, mostly. And I came out at the other end of the tunnel (winter) quite renewed and feeling fresh, which of course is nature's intention for itself including us diabetics. I post a picture of the 'new' and inspired and motivated me and greet you with all my heart and love.
If you read this blog and post, plese post me your diabetic status and any problems in the management of your blood sugar in the comments section, so I can concentrate on helping you along with my research and efforts. Thank you and have a wonderful season, whatever this might be the case in your country!
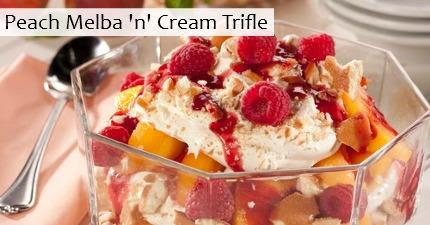
I quickly add a photo -along the lines of, when the heart is full of something nice, it runs over- of the only one in my home who MAY it sweets......
So here goes:
Blood sugar checks, eAG readings, calorie counting — if you’re living with
type 2 diabetes, you know that the successful management of the condition can be a numbers game. One of the most important numbers to keep tabs on is your A1C.
The A1C test result reflects your average blood sugar (glucose) level over the previous two to three months, enabling you and your doctor to gauge your blood sugar control over a long period, as compared with your daily self-checks, which provide one-time pictures of your fluctuating
blood sugar level. The American Diabetes Association (ADA) compares the A1C test to a baseball player’s batting average — it gives you a more accurate view of your overall success in managing type 2 diabetes.
Getting an A1C test — which should be performed at your doctor’s office two to four times a year — is important because the results can help you and your doctor determine if your type 2 diabetes treatment strategy is working. If your test results don't measure up, the two of you can make changes to your plan to help you gain better control over your blood sugar levels and prevent the long-term complications of type 2 diabetes.
The A1C test also reduces the risk of error associated with blood sugar self-monitoring. “People sometimes use glucose monitors inaccurately or incorrectly,” says
Derek LeRoith, MD, PhD, a professor of medicine, endocrinology, diabetes, and bone disease at the Icahn School of Medicine at Mount Sinai Hospital in New York City. “We can look at both the A1C results and the chart that a person brings in to see if there’s a discrepancy.”
What Do Healthy A1C Results Look Like?
According to the National Institute of Diabetes and Digestive and Kidney Diseases, a person who doesn't have type 2 diabetes probably has an A1C level somewhere between 4.5 and 6 percent. Although your doctor will determine your personal target, people with type 2 diabetes often aim for an A1C level of 7 percent or less. A level of 8 percent or higher indicates uncontrolled type 2 diabetes.
What does the A1C test actually measure? Dr. LeRoith explains that hemoglobin is a protein that’s found in red blood cells. When glucose is in the bloodstream, it coats the protein with sugar — a process known as glycation. The A1C test measures the percentage of your hemoglobin that is glycated to help determine your blood sugar control.
It can also be helpful to know your estimated average glucose level (eAG). This is essentially the same as your A1C test result, except that the value is converted to the unit (mg/dl) that you see when you self-check your blood sugar level at home. If you’re aiming for an A1C result of less than 7 percent, you’re also shooting for an eAG that’s below 154 mg/dl. The ADA provides an
online tool that converts your A1C level to eAG and vice versa.
8 Ways to Lower Your A1C
It’s important to remember that lowering your A1C level takes time — the length of time it takes you to do it depends on your current blood sugar levels and
lifestyle habits. Because the reading represents an average level over two to three months, you won’t be able to lower your A1C by going on a 20-minute jog just before your appointment.
However, if your previous reading wasn’t in a healthy range, there are things you can do to lower your A1C before you see your doctor again. Try these tactics:
Follow your doctor’s orders. If your last A1C test result was too high, it's a sign that you’ve lost some degree of control. “To reach a target A1C, the person with type 2 diabetes and his or her doctor must address overall blood sugar management,” LeRoith says. “That could mean losing weight,
increasing fitness, or making medication changes.” No matter what the plan requires, the most important part is sticking to it.
Eat healthier foods every day. “I don’t put people with type 2 diabetes on strict diets,” says Gregory Dodell, MD, an endocrinologist in New York City. “Instead, I come up with an overall healthy eating plan with them. I remind them, 'This is something you’re going to be changing for the rest of your life.'”
According to the ADA, healthy eating plans that help with blood sugar control make room for a wide variety of foods, including vegetables, lean meat, fish, whole grains, fruits, and nonfat dairy products — and yes, even the occasional dessert.
When you’re changing the way you eat overall, it’s okay to start small. “Do you love rice? Switch from white rice to brown rice,” Dr. Dodell says. Your doctor or a registered dietitian can work with you to set realistic dietary goals.
Be label conscious. “Most people just look for calories on food labels,” LeRoith says. “People with type 2 diabetes also need to be looking at the nutrition — most importantly, added sugars.” Since healthy eating plans that lower blood sugar incorporate nutrient-rich foods, the ADA recommends checking labels for total carbohydrates, fiber, total fat, sodium, and sugar alcohols.
Develop an exercise habit. The ADA recommends that people with type 2 diabetes aim to get 30 minutes of moderate- to high-intensity exercise at least five days a week. Exercise is good for everyone, but it can help people with type 2 diabetes gain control over their blood sugar level and their weight.
If you don’t currently have an exercise routine, you don't have to go from 0 to 60. “Let’s say you don’t like to run but you enjoy walking,” says Dodell. “Could you start off by walking for 10 minutes three times a day? Can you get off the train a stop early and walk the rest of the way? It’s all about coming up with a realistic plan.”
LeRoith agrees that walking is a good first step. “Any exercise will work, but walking is great for two reasons. First, many people with diabetes don’t walk as much as they should. Second, walking generally causes less harm to the back, legs, and other body parts compared with more intense exercises.”
Keep tabs on your blood sugar level at home. Even though your doctor is testing your A1C every few months, it’s still important that you do frequent self-checks — and keep track of your results — at home. Says LeRoith, “Testing blood sugar only once every three months is just too late.”
LeRoith also stresses the importance of testing after meals (as opposed to testing only your fasting glucose level in the morning). “This helps you see how well you’re coping with the meal,” he says, “and how important it is to reduce the sugar in your meals.” Keeping tabs on your blood sugar readings at home can help you gauge whether you’ll be in your goal A1C range by your next appointment — and whether you need to make diet and fitness adjustments to get there.
Get techy with your tracking. If you have a smartphone, you’re in luck. There are a number of apps designed to help you gain better control over your type 2 diabetes.
Glooko and
BG Monitor Diabetes, for example, enable you to keep track of your blood sugar readings and to analyze your data, allowing you to better estimate what your A1C will be before you see your doctor.
Weight-loss apps such as
Lose It! can assist with weight management, and Everyday Health’s
Diabetes in Check comes with a carb tracker and built-in diabetes coach. Smartphone apps, LeRoith says, are effective tools in helping you be as prepared as possible for your next doctor’s appointment.
Try to reduce stress. Everyone gets stressed out, but if you can possibly reduce the amount of stress in your life, you may be able to better manage your blood sugar — and ultimately lower your A1C level. The ADA explains that when we suffer mental or physical stress, our bodies release hormones that make us less sensitive to insulin — consequently, blood sugar increases. Adopting long-term stress-reduction techniques (like practicing yoga once a week, exercising more often, or adding deep-breathing exercises to your day) may help you lower tension and your A1C.
Focus on the big picture. “Even when someone’s type 2 diabetes is uncontrolled, they may feel fine and not have any symptoms,” Dodell says. “They may say, ‘I feel okay, so I’m going to keep on doing what I’m doing.’ I then tell them, ‘Look, this is preventive.’” He advises that you make an active decision to get your A1C to a healthy range to protect your future health. Making healthy lifestyle tweaks today can help you prevent complications of type 2 diabetes — such as stroke, kidney disease, blindness, and amputation — down the road.
Not Seeing Improved A1C Results?
If you feel as though you’ve been doing everything right but you're still not hitting your A1C target, try not to get discouraged, LeRoith says. “At that point, your doctor will reevaluate your treatment plan and what’s not working — whether it might be diet or exercise. Then he or she will talk about medication.” If you’re already on medication, your doctor may increase the dosage or add another medication.
Together, you and your doctor — along with the aid of some healthy lifestyle modifications — can get your blood sugar level down to a healthy range.